How the clinical application of Yoga Therapy can help with Strokes and Traumatic Brain Injury

Evi Dimitriadou, presents the rehabilitation she undertook for 6 months and for four hours a day with a patient after a Traumatic Brain Injury (TBI). Traumatic Brain Injury and Stroke have very similar rehabilitation guidelines we hope that this article can show you how much the clinical application of yoga therapy can help.
Although research articles suggest that continued recovery is possible (Freund et al., 2013), systematic reviews recommend intensive therapeutic practice for TBI within one year of diagnosis (Miyai et al., 2009) with the recovery having the tendency to slow down after the first 6 months reaching highest functional plateau by 12 months (Walker and Pickett, 2007).
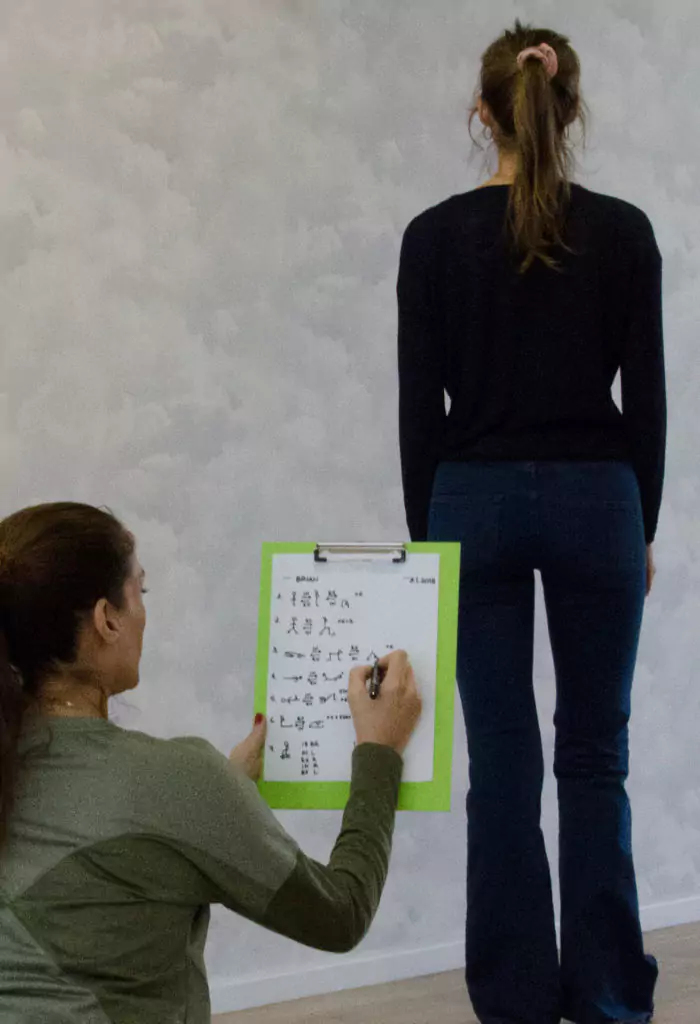
Keeping well detailed records of the daily practices with the exact exercises, of the intensity, of the steadily increased number of repetitions and of the length of time staying performing the exercises and standing upright, was very important in monitoring the patient’s progress and the program’s effectiveness.
The main symptoms were aphasia (difficulty to communicate), nystagmus (tendency to keep falling asleep), headache (may last 6-12 months), reduced sharpness of vision, left hemiparesis (loss of sensation and movement at the specific side) and ataxia (uncoordinated movement), hypostatic hypotension (low blood pressure in standing) which are common signs of TBI and cerebellar dysfunction (Stephen et al., 2019).
The short-term goals were to gain body proprioception (awareness of the body in terms of space) and coordination, balance in the sitting position as well as to be able to stand with minimum support within 2 months while the long-term goals were to walk in 6 months. Goals that were achieved through an intensive program of 4 hours per day since international guidelines such as the Brain Injury guidelines by the Ontario Neurotrauma Foundation recommend at least 3 hours of rehabilitation program by a multidisciplinary team.
The goals were reached due to the program’s included task-oriented activities such as sit-to stand (up to 100 utkatasanas per day) and treadmill training, movements for upper and lower limb (many variations of dwipada pitham, jatthara parivritti, apanasana, supta padangustaana, supta badha konasana) on a bobath bed, after the first 2 months more standing practices (small virabadrasana I, tadasana) at an increasingly larger number of repetitions and length of stay within each session, since repetitions play a crucial role in neuroplasticity (Kimberley et al., 2010). The patient regained the body coordination, the sitting position, the standing and the walking ability due to the customized physiotherapy program which focused on retraining proprioception and coordination using visual and sensory stimuli (cues) by showing, touching and communicating constantly with the patient.
Although different people need different treatments and some people need different services in different phases of their rehabilitation (Turner-Stokes and Wade, 2004) what is common and crucial based on research on neuroplasticity (the ability of creation of new synapses/communication paths within the brain at any age and condition) is the need for an intensive, creative and customized practice. Every person is unique, and this is the reason that rehabilitation is suggested to be customized as yoga therapy is.
#yogatherapy #stroke #rehabilitation #yogatherapygreece #traumaticbraininjury #intensiveprogram #customizedyogapractice #yogaandrehabilitation