The role of Yoga Therapy in Pain Management Programs

Yoga has a lot to offer individuals challenged by pain and in particular for chronic pain conditions. As C-IAYT Yoga Therapists we know this. Through this article, we explore how and why Yoga Therapy can be part of Pain Management Programs.
What is Pain?
According to International Association of the Study of Pain (IASP), Pain is a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
Pain depends on our brain’s evaluation of danger and the likely benefit of protective behaviour. But Pain is also perceived because our brain is convinced that our body needs protecting.
The development of chronic pain is the result of a dynamic interaction between physical, psychological and social factors. These contribute to the experience of chronic pain and shape the individuals cognitive, emotional and behavioral responses to the pain (Turk and Flor 1999). These factors contributing to pain, become established behaviours with chronicity, the so-called pain behaviours.
Pain behaviours such as altered posture and movement, verbal complaints, fear avoidance are suggesting pain but also fear of movement due to pain or the possibility of pain, psychological distress and low self-efficacy, although patients are not conscious of these behaviours (Harding and Watson, 2000).
By Addressing the cognitive and the emotional aspects of chronic pain, self-efficacy and perceived control over pain is increased, the catastrophizing thinking and the hypervigilance is decreased, pain density, function and symptoms are improved. (Adams and Turk, 2018).
The Biopsychosocial Approach
The need to address the biological/physiological, psychological, and social factors which underline and may even aggravate the clinical symptoms in chronic pain conditions gave rise to the contemporary biopsychosocial (BPS) model in medicine and physiotherapy. The approach aims at all these factors contributing to the chronic pain perception and disability of the individual (Waddell, 2004).
The BPS is a patient-centred approach where the patient’s characteristics such as thoughts, beliefs, behaviours, expectations, and way of life will determine the intervention and shape the characteristics of the exercise treatment approach (Meeus et al., 2016).
The BPS framework suggests that patient’s goals besides being the priority should be realistic, enjoyable, physical regarding the physical activity and exercise, functional regarding their daily life activities, psychological (cognitive and effective) and social, depending on the individual’s needs (Booth et al., 2017).
The BPS approach is the most effective approach for chronic pain management per se, (Meeus et al., 2016) is well established and more effective than exercise or physiotherapy alone for CLBP (Kamper et al., 2015) and should underline the Pain Management Programs (PMPs) for chronic pain conditions.
The key points for prescribing exercise/movement taking into account the biopsychosocial approach/model are:
To be specific to the individuals (individualized), to be of graded low to moderate intensity, the exercise programs to be supervised in order to improve adherence in manageable portions that do not aggravate the symptoms and should be based on the patient’s goals and preferences (Booth et al, 2017).
This is exactly what yoga therapy does and not only in terms of exercise.
Also, it is very important to monitor and provide constructive feedback on the way the individuals practice and to recommend ways patients self-monitor in order to enhance exercise participation (Moseley, 2006), to have prepared responses to possible flare ups in order to feel safe, to stay as active as their symptoms allow and to develop confidence and quality in the way they move (Booth et al., 2017).
This is exactly what we do in yoga therapy.
It is also very important to explain how the muscles engage in every exercise and the reason for the selection of this movement, while the choice of the specific exercises for the individual is made based on the movements that aggravate and relieve patients as well as the level of function of the individual.
If by all means the symptoms are aggravated, then pacing the daily physical activities with no exercise is recommended (Booth et al., 2017).
This is exactly what we do in yoga therapy.
What Pain Management Programmes are?
According to the Medical World, leading Physiotherapists, NICE guidelines, British Society of Pain and WHO the Pain Management Programmes (PMPs), based on cognitive behavioural principles, aim to reduce the disability and distress caused by chronic pain by educating patients ways to cope with physical, psychological and social aspects of life improving overall quality of life.
Pain Management Programmes in public and private healthcare are offered to individuals showing distress, disability and negative effect on their quality of life due to any chronic pain. In this setting they are be implemented by psychologically informed health professionals and by interdisciplinary teams – specialists from different background sharing the biopsychosocial approach
The common goals of pain management/pain care are:
Less pain, better ease of movement/function and enhanced quality of life.
The principal aim is on better function, achieving as normal a life as possible by shifting the focus of the individuals from pain to personal goals reducing the effects of pain, emotional distress and physical disability (Harding and Watson, 2000).
Pain Management/pain care includes medical care, pharmacological care and
non-pharmacological care (exercise, physiotherapy, cognitive therapies, yoga therapy, etc).
Standard PMP consist of 12 half day sessions and is given mostly in groups of 8-12 by an interdisciplinary team sharing and using cognitive behavioural principles. They are classified as intensive, standard and stratified to risk.
The most effective pain management programs, highly recommended in chronic pain conditions consist of graded person-centered exercise, cognitive therapies and pain Education that enhance acceptance, mindfulness and psychological flexibility as well as relaxation, self -management and pacing of overall activities (British Pain Society, 2013). Tailored made to individuals needs and capabilities advice and information to enhance self-management is highly suggested by the National Institute of Health and Excellence (NICE, 2016). Also, diaphragmatic breathing, autogenic relaxation, repetition of positive affirmations and guided imagery relaxation/visualization are also highly recommended for their effects on balancing the nervous system by shifting to parasympathetic activity and giving a sense of control as well as enhancing pain self-management (Harding and Watson, 2000, O’Sullivan, 2018).
There are many effective ways to implement BPS approach and have a behavioural change in Pain Management Programs, such as Cognitive Behavioural Therapy (Veehof et al., 2011), the Acceptance and Commitment Therapy (Hughes et al., 2016), the Mindfulness-based therapies (Kabat-Zinn, 2005),) the Cognitive Functional Therapy (O’Sullivan et al., 2018), the Pain Neuroscience Education (PNE) (Moseley, 2002), etc.
What about Yoga Therapy?
Yoga therapy as a patient centred holistic mind and body intervention share many common elements with mindfulness-based stress reduction, cognitive behavioural therapy and acceptance-and-commitment therapy (which includes pain acceptance and psychological flexibility) while it incorporates movement.
As Yoga Therapists we have the skills to build a long-term therapeutic relationship that facilitates information enhancing self-management strategies, to motivate patient preferred physical activities and movements that address the needs of the individual and lead to lifestyle changes. Through the long-term relationship we are able to monitor the progress, the adherence and the outcomes but also to provide constructive feedback and necessary adjustments of the self-management programs.
We always explain the meaning of the practice given, of the movement explored or practice suggested, making them feel safe to move and engage in personal practice despite their symptoms and some discomfort due to a possible deconditioned system.
In yoga therapy we apply the biopsychosocial model, the pancamaya kosha model, the patient centred approach, taking into consideration the personal needs and capabilities, the differences in body, mind, energy level and spirit, promoting mindfulness, compassion, commitment and acceptance.
During the intake we connect with the clients and we have the time to assess the habits, the needs, the goals of the individual, to assess the breath and the body, and together explore movements that help people regain movement, release tension, facilitate breath, shift their attention from pain, change the story that plays in their mind about pain, make them feel better and gradually increase their quality of life.
We address the stories that continue unchecked and unquestioned within them and which during yoga practice when pain persists can become barriers to recovery.
We focus on shifting attention e.g. knowledge and understanding about the state of the tissues or meditation practices that direct attention elsewhere in the body; or treatment can be directed to the painful part. e.g. graded exposure to movement or touch of the painful body part so that the person can get more comfortable with the body parts in pain.
In yoga therapy we start with the Anamaya kosha taking into consideration the body’s needs and capabilities (anamaya kosha), the personal energy level, the function/physiology and the condition of the nervous system that is expressed by the breath and the way people sleep (pranamaya kosha), the way people think about their condition and the effect of pain in their life (manamaya kosha), their characters/personalities and the way they relate to family, society (vijnamaya kosha) and what supports them and makes them feel happy (anandamaya kosha).
Pain also interacts with the gunas (the attributes of life), is affecting the agni and functioning of all systems showing how people live with pain when it persists. In a persisting pain situation, our elements (bhuta) can be pushed into increasingly greater imbalances pushing us into our vikruti (disordered) dosha.
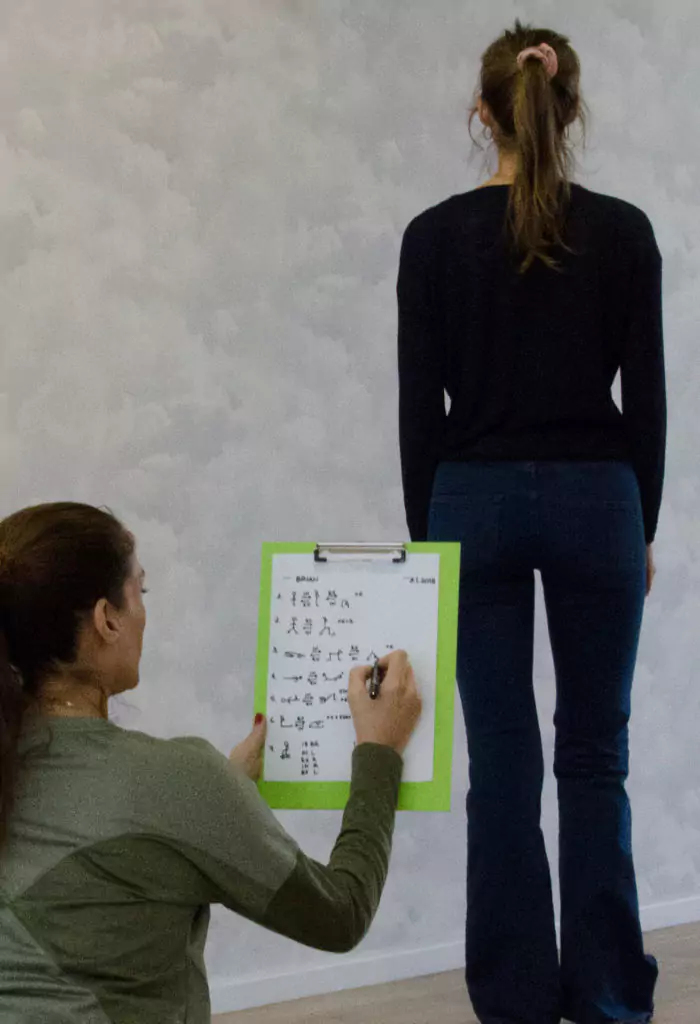
Through the structural and movement assessments during the first session and the careful supervision in each session, collaboratively with the participant, we assess for musculoskeletal symptoms and signs, we facilitate the individual to gain body awareness, to explore and regain movements and physical activities that may have been challenged due to pain and we develop effective practices with movements/asanas, breathing/pranayamas and relaxations that will restore the physical function and as a result improve the individual’s quality of life. We match practices with the changes seen in someone’s physiology & awareness.
And then we proceed with the client to the development of a personalized yoga practice that may consist of modified asanas, pranayamas, restorative postures, guided relaxation, meditation, body scan, yoga nidra, humming/chanting etc.
Pain Education
What we may need to add in our Yoga Therapy practice is pain education of the client that may make it easier to shift non-productive and self-limiting beliefs.
Pain Education of patients can start at the first appointment in order to make an informed decision to do their home yoga therapy practice/ to actively participate in the intervention or self-management program that is ultimately leading to cognitive reappraisal and behavioural change, which is the main goal (Bettie et al. 2016, O’ Sullivan et al. 2018, Harding and Watson, 2000).
We also talk about the fact that everything is changing, our thoughts, our life, even the perception, the quality and the intensity of pain and we help in developing mental/behavioural flexibility.
We educate and we make allowances for some initial increase in discomfort after practicing in cases where people have been inactive for some time. We try to normalize a potential initial discomfort/pain response.
Strategies for Pain Education
Ways to educate/to achieve a conceptual change regarding pain experience.
- Honour the client.
- Ask them what they know about their problem, what do they know about their diagnosis, whether they have any theory about what is causing the pain, how do they think you can help them?
- De-threaten diagnosis and radiology reports, affirm and enhance the correct concepts (that enhance safety) and remove the unhelpful ones (the ones that promote danger), congratulate their wise body for the protection it offered so far.
- Present an alternative concept and some easy short-term evidence-based statements that helps reconceptualize the experience of pain. For example; Exercise is no longer for me versus we know that age does not link to pain. My disc is flat versus you can inflate it with exercise, time and understanding. I have slipped disc versus it is extremely difficult to have a slipped disc being so firmly connected to the bones with strong ligaments. I have degenerative discs versus of people over fifty 90 % have disc degeneration but have no pain & 90% of people with pain have no identifiable reason.
- Empower them. ‘You know that you can influence the perception of pain, that you are stronger than any pain killer if you rest, move, breath, relax (meditate) and do things that you like’.
- Use metaphors such as motion is lotion, use the painkillers of your brain
- Avoid catastrophizing language.
- Stress the importance of good habits such as enough sleep, of relaxation, of breath, of less alcohol, of less caffeine etc.
- Support them with the integration of good habits in their everyday life.
It is obvious so far that yoga therapy is by itself a very effective patient centred pain management intervention. Yoga Therapists having the appropriate biomedical pain education can offer an even better pain management program or be part of an interdisciplinary team supporting people challenged by pain.